This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This is a case of a 56 year old female who is a lemon seller by occupation hailing from Chityal who came with complaints of
1. Nausea and 2 episodes of vomiting since 1 day
2. Breathlessness since 8 days
3. Pain abdomen and fever since 10 days
HISTORY OF PRESENTING ILLNESS
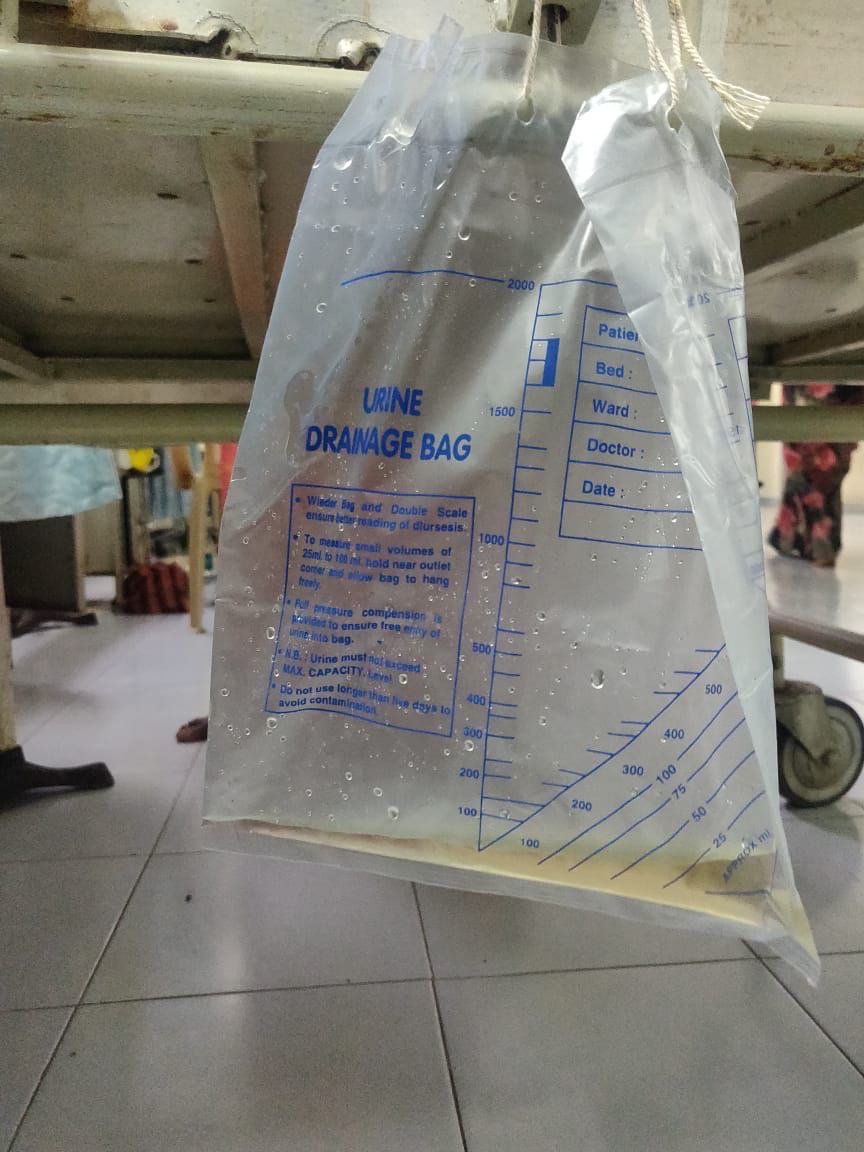
The patient was apparently asymptomatic 10 days back. Then she developed fever which was insidious in onset, intermittent low grade associated with chills and rigours. Fever was associated with dry cough with scanty white coloured sputum for the first 2 days. She also noted she had decreased urine output since 10 days. No history of vomiting, loose stools, burning micturition at that time.
The patient later developed pain abdomen which was insidious in onset and gradually progressive. She localised the pain to her right upper quadrant. It was sharp in nature non radiating. There are no aggravating and relieving factors. In the initial days, the pain was bearable but later it was too severe for her and was hindering her daily activities.
2 days later after the fever developed she developed shortness of breath. Initially of grade 2 (NYHA classification) - slight limitation of activity -ordinary activity results in fatigue. Which aggravated to grade 3 at present (marked limitation of physical activity- less than ordinary activity causes dyspnea). Not associated with orthopnea and PND.
She was taken to a local hospital by her family 5 days after the onset of fever. She was prescribed some medication that included antibiotics and antipyretics and was brought back home. The fever and the cough subsided for 3 days but then the fever progressed again and her breathlessness was still present. She was taken to the hospital again as was prescribed medication. She claims to be fine for 2 days, but her pain became unbearable and she also had an episode of vomiting, watery in consistency about 100 mL with no food particles, non bilious, non blood stained. She also had generalised weakness and was not able to walk around. She was then brought to our hospital. After arriving she had a similar episode of vomiting.
PAST HISTORY
The patient developed cellulitis 3 months ago on her right leg up to her knee. She consulted a local practitioner and was given an injection in her left buttock. She then developed a hard mass in her left gluteal region. As she has been lying down and resting because of her ailment, it has ulcerated the past 10 days.
No history of similar complaints in the past or previous hospitalisations(Telma)
The patient was diagnosed with hypertension 2 years ago during a regular checkup. Since then she has been on regular medication.
PERSONAL HISTORY
Daily routine:
The patient lives with her husband and her son’s family. Her attenders say that she is an active lady and does all her daily chores without assistance. She wakes up at 6 in the morning and freshens up. At 7 she has breakfast consisting of rice and curry. At 8 she gets ready and goes to the local market to sell lemons. She sits down and sells lemons the whole day at the market. She takes a lunchbox and has her lunch there which again consists of rice and curry. Around 5 or 6 she comes back to her house. She uses an auto for transportation while going and coming. She usually chats with her family members for some time and does her daily chores.
She has dinner at 8 and goes to bed at 10.
The past few days however she has only been consuming liquid food such as porridge and has not been going to the market to sell lemons.
Diet: mixed
Appetite: Decreased since 10 days
Sleep: adequate
Bowel and Bladder: Stool content have decreased and infrequent micturition
Habits: She drinks toddy regularly since the past 20 years. Since the past 5 years she has been consuming alcohol 15-30 mL twice or thrice a week depending on her mood. She admits cravings for alcohol. Last time she consumed alcohol was before she developed fever
FAMILY HISTORY
Not significant
CLINICAL EXAMINATION
I have examined the patient after taken prior consent and informing the patient in the presence of a female attendant. The examination was done in both supine and sitting position in a well lit room.
The patient was conscious coherent and cooperative. Well oriented to time place and person. Well built and nourished.
No pallor, cyanosis, clubbing, lymphadenopathy or edema
Icterus is present
Truncal obesity is seen
Patients hands with a comparison with my hand
Icterus seen(may not be visible in the below photo due to light)
Vitals:
Pulse - 90 bpm
BP - 140/80 mm Hg
RR - 22 count
Temp- 97.6 oC
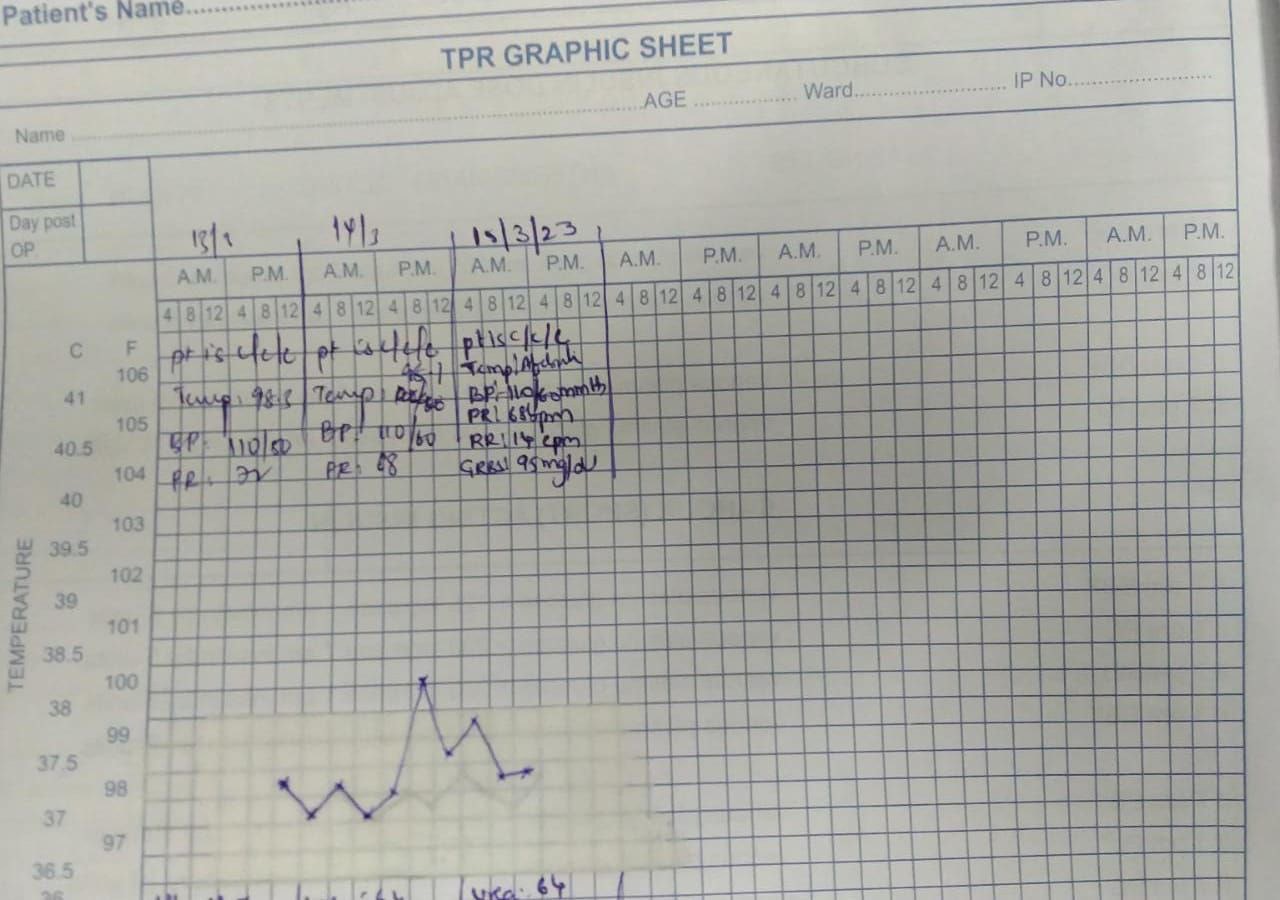
FEVER CHART
SYSTEMIC EXAMINATION:
PER ABDOMEN
INSPECTION
➤Shape - round, large with no distention.
➤Umbilicus - Inverted
➤Equal symmetrical movements in all the quadrants with respiration.
➤No visible pulsation,peristalsis, dilated veins and localized swellings.
PALPATION
➤Superficial :Local rise of temperature in right hypochondrium with tenderness
also noted in epigastric region
and localised guarding and rigidity.
➤ DEEP :
Enlargement of liver, regular smooth surface , roundededges soft in consistency, tender, moving with respiration non pulsatile
➤No splenomegaly
➤Abdominal girth : 105 cm
➤xiphesternum to umbilicus distance-22 cm
umblicus to pubic symphysis - 14 cm
PERCUSSION
➤Hepatomegaly : liver span of 14 cms with 4 cms extending below the costal margin
➤Fluid thrill and shifting dullness absent
➤puddle sign not elicited as patient was not willing
AUSCULTATION
➤ Bowel sounds present.
➤No bruit or venous hum.
LOCAL EXAMINATION Of LEFT GLUTEAL REGION
On inspection 3x4 cm,margins are well defined,edges are slopping and floor has Slough and granulation tissue
NO DISCHARGE PRESENT
CVS:
Inspection:
There are no chest wall abnormalities
The position of the trachea is central.
Apical impulse is not observed.
There are no other visible pulsations, dilated and engorged veins, surgical scars or sinuses.
Palpation:
Apex beat was localised in the 5th intercostal space 2cm lateral to the mid clavicular line
Position of trachea was central
There we no parasternal heave , thrills, tender points.
Auscultation:
S1 and S2 were heard
There were no added sounds / murmurs.
Respiratory system:
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS:
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION
Normal sensations felt in all dermatomes
MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
DIFFERENTIAL DIAGNOSIS:
Viral hepatitis
Liver abscess
NASH
Alcohol hepatitis
Cholecystitis
Cholelithiasis
INVESTIGATIONS:
1)USG abdomen:
Findings- 5 mm calculus noted in gall bladder with GB sludge
Impressiom- Cholelithiasis with GB sludge
Grade 2 fatty liver with hepatomegaly
2)RFT:
13th
Blood urea 58 mg/dl
Sr creatinine 1.9 mg/dl
serum Na 127 mmol/dl
Serum K 3.4 mmol/dl
Serum Cl 92 mmol/dl
14th
Blood urea 64 mg/dl
Sr creatinine 2.1 mg/dl
serum Na 117 mmol/dl
Serum K 3.4 mmol/dl
Serum Cl 70 mmol/dl
15th
Blood urea 64 mg/dl
Sr creatinine 1.6 mg/dl
serum Na 125 mmol/dl
Serum K 3.0 mmol/dl
Serum Cl 88 mmol/dl
3)LIVER FUNCTION TEST:
14th
Total bilirubin:2.6* mg/dl
Direct bilirubin: 1.1* mg/dl
Indirect bilirubin:1.5* mg/dl
Alkaline phosphatase:193* IU
AST:37 IU
ALT:21 IU
Protein total: 7.0 G/DL
Albumin:4.3g/dl
Globulin:2.7 g/dl
Albumin and globulin ratio:1.6
4)CUE:
Albumin:+
Sugar: nil
pus cells:3-6 /hpf
epithelial cells-2-4 /hpf
urinary na 116 mEq
urinary k 8 mEq
urinary cl 128 mEq
5)Arterial blood gas:
Pco2: 23.3 mmHg
PH: 7.525
Hco3: 23 mEq/L
Po2: 80.8 mmHg
6) x ray Abdomen
7)complete blood picture:
13-3-23
Haemoglobin:11.7 g%
Red blood cells:3.81 million/mm3
Pcv:32.5 %
Platelet count:5.0 lakhs/mm3
Total leucocyte count:22,400 /mm3
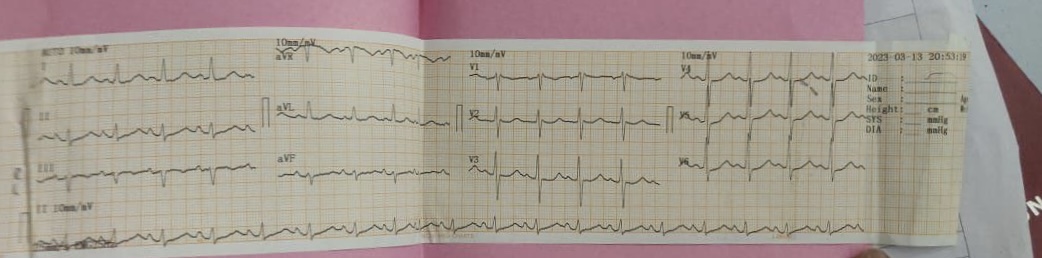
8)ECG:
PROVISIONAL DIAGNOSIS:
Acute Cholecystitis
AKI secondary to sepsis
TREATMENT PLAN
1. Liquid diet
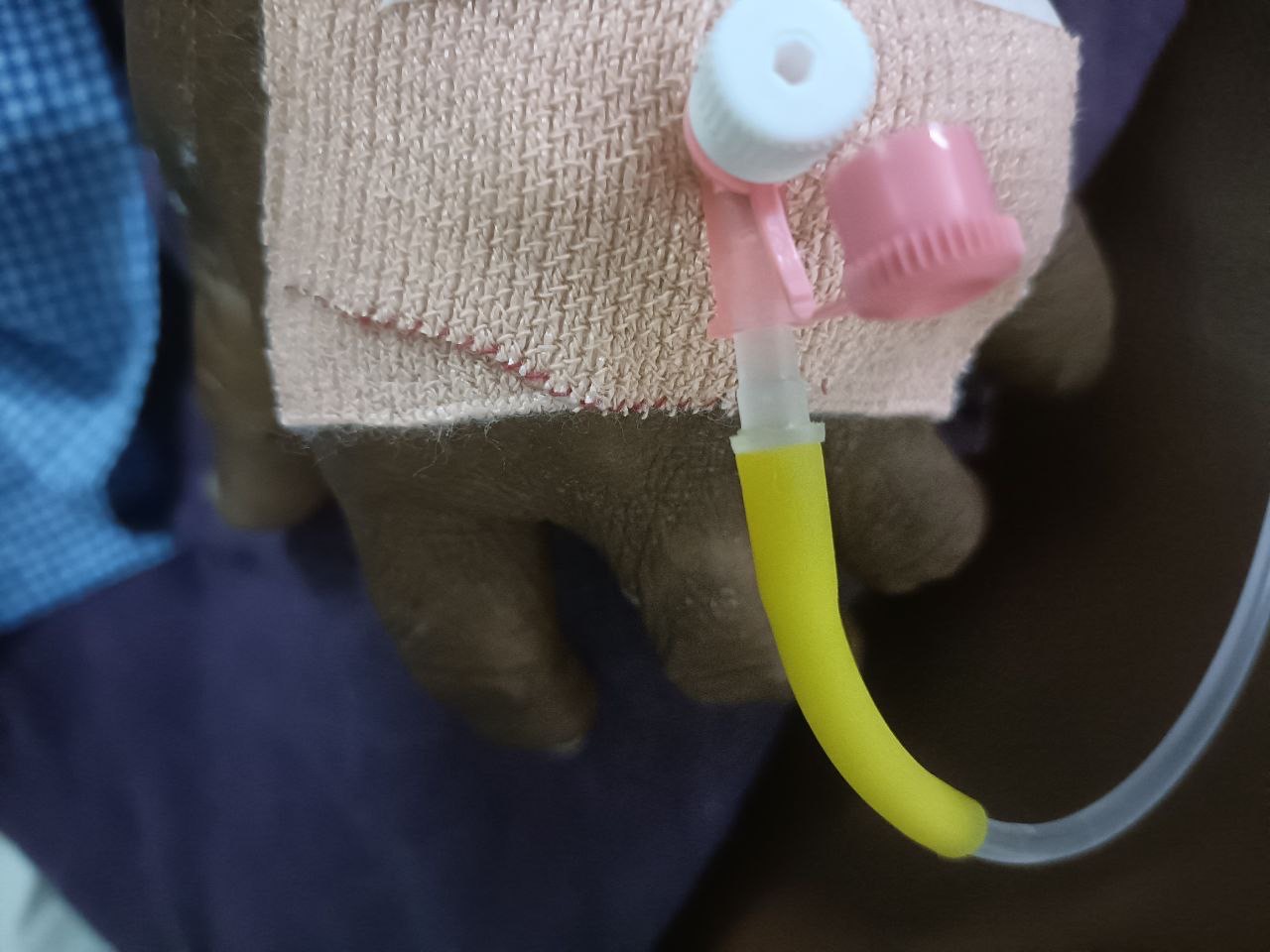
2. Iv fluids 1 unit NS, RL, DNS 100 ml/hr
3. Inj PAN 40 mg iv/ od
4. Inj PIPTAZ 2.25mg/iv/TID
5. Inj. METROGYL 500mg / iv/tid
6. Inj zofer 4mg iv/sos
7.INJ NEOMOL 1gm iv/sos
8.T.PCM 650mg po/tid
9.T.CINOD 10mg po/od














Comments
Post a Comment