This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This is a case of a 30 year old male, carpenter by occupation came to casualty with chief complaints of:
Pain in abdomen since evening(26-5-23)
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 month ago then he developed pain in the abdomen- in epigastric region.
It was sudden in onset, gradually progressive.
Pain more after eating food (especially spicy food) and on lying in supine position
Pain relieved on medication
At present, patient came with complaints of pain abdomen in epigastric region non radiating since evening
No SOB, palpitations, orthopnea, PND.
No c/o fever, vomitings, diarrhea.
Last binge of alcohol consumption 2days ago
PAST HISTORY:
Not a K/C/O DM, HTN, TB, Asthma, Epilepsy,CVA,CAD
PERSONAL HISTORY:
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder regular
Consumes 2quarters of alcohol/day.
FAMILY HISTORY
No significant family history
GENERAL EXAMINATION
Patient is conscious , coherent and cooperative. Well oriented to time place and person.
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
BP-130/80mmhg
PR- 96 bpm
RR- 18cpm
GRBS- 104 mg/dl
Temp- 98.2F
SYSTEMIC EXAMINATION
PA:
Inspection:
Scaphoid
Umbilicus: Inverted
No visible pulsation,peristalsis, dilated veins and localized swellings.
Palpation:
Soft, tenderness present in epigastric region
No signs of organomegally
Percussion:
No fluid thrill, shifting dullness absent
Auscultation:
Bowel sounds heard
CVS:
Inspection:
There are no chest wall abnormalities
The position of the trachea is central.
Apical impulse is not observed.
There are no other visible pulsations, dilated and engorged veins, surgical scars or sinuses.
Palpation:
Apex beat was localised in the 5th intercostal space 2cm lateral to the mid clavicular line
Position of trachea was central
Auscultation:
S1 and S2 were heard
There were no added sounds / murmurs.
RESPIRATORY SYSTEM:
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS:
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION
Normal sensations felt in all dermatomes
MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
CLINICAL IMAGES
INVESTIGATIONS
AMYLASE 26
LIPASE 40
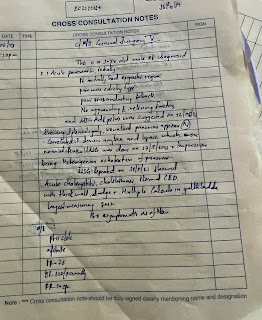
SURGERY REFERREL
Diagnosis- ?acute pancreatitis
Treatment-
1.NBM till further orders
2.IV NS, RL, DNS at 100ml/ hr
3.Inj. Pan 80mg in 100ml NS IV over 1 hour
SOAP NOTES
27/05/2023
Ward :ICU
Unit : 5
DOA : 26.5.2023
30 year male with epigastric pain
S
C/O pain abdomen
No fever spikes
Stools passed
O:
Patient is conscious coherent and cooperative
No pallor, icterus ,clubbing,cyanosis,lymphadenopathy ,pedal edema
Vitals :
BP- 130/80 mmhg
PR -82bpm
RR-16cpm
Spo2-95% at room air
Temperature - 98.5F
CVS: s1,s2 heard ,no Murmurs,jvp not raised
RS:BAE,no added sounds ,NVBS,
P/A: soft, distended, tenderness
CNS:NFND
A:
Pain abdomen under evaluation
? Acute gastritis
? Acute pancreatitis
P:
1. NBM till further orders.
2. IVF- NS, RL, DNS at 100ml/hr
3. Inj. Pan 80mg in 100ml NS / IV over 1 hour
4. Monitor vitals 2nd hourly
5. I/O charting
6. GRBS 4th hourly
28/05/2023
Ward :AMC
Unit : 5
DOA : 26.5.2023
30 year male with epigastric pain
S
C/O pain abdomen decreased compared to yesterday
No fever spikes
Stools not passed
O:
Patient is conscious coherent and cooperative
No pallor, icterus , clubbing, cyanosis, lymphadenopathy , pedal edema
Vitals :
BP- 120/70 mmhg
PR -94bpm
RR-16cpm
Spo2-95% at room air
Temperature - 98.7F
I/O:2100/1050ml
GRBS at 8:00am: 113mg/dl
CVS: S1,S2 heard ,no Murmurs, jvp not raised
RS:BAE,no added sounds ,NVBS,
P/A: soft, distended, tenderness present
CNS:NFND
A:
Acute pancreatitis
P:
1. NBM till further orders.
2. IVF- NS, RL, DNS at 100ml/hr
3. Inj. Pan 40mg IV BD
4. Inj. Tramadol 1amp in 100ml NS IV/ BD
5. Inj. Thiamine 200mg in 100 ml NS IV/ TID
6. Monitor vitals 4th hourly
7. I/O charting
8. GRBS 4th hourly
29/05/2023
Ward :ICU
Unit : 5
DOA : 26.5.2023
30 year male with epigastric pain
S
C/O yellowish discolouration of urine
C/O R hypochondriac region pain (tenderness +)
No fever spikes
Stools not passed
O:
Patient is conscious coherent and cooperative
No pallor, icterus ,clubbing,cyanosis,lymphadenopathy ,pedal edema
Vitals :
BP- 120/80 mmhg
PR -96bpm
RR-18cpm
Spo2-95% at room air
Temperature - 98.4F
GRBS at 8:00am 107 mg/dl
CVS: s1,s2 heard ,no Murmurs,jvp not raised
RS:BAE,no added sounds ,NVBS,
P/A: soft, distended, tenderness
CNS:NFND
A:
Acute pancreatitis
P:
1. NBM till further orders.
2. IVF- NS, RL, DNS at 100ml/hr
3. Inj. Pan 40mg IV BD
4. Inj. Tramadol 1amp in 100ml NS IV/ BD
5. Inj. Thiamine 200mg in 100 ml NS IV/ TID
6. Monitor vitals 4th hourly
7. I/O charting
8. GRBS 2nd hourly
30/05/2023
Ward :AMC
Unit : 5
DOA : 26.5.2023
30 year male with epigastric pain
S
C/O yellowish discolouration of urine
C/O epigastric pain
1 fever spike
Stools not passed
O:
Patient is conscious coherent and cooperative
No pallor, icterus , clubbing, cyanosis, lymphadenopathy , pedal edema
Vitals :
BP- 120/80 mmhg
PR -90 bpm
RR-18 cpm
Spo2- 98 %at room air
Temperature - 98.2
GRBS at 8:00am -124mg/dl
CVS: S1,S2 heard ,no Murmurs,
RS:BAE,no added sounds ,NVBS,
P/A: soft, non tender , no organomegaly
CNS:NFND
A:
Acute pancreatitis
P:
1. NBM till further orders.
2. IVF- NS, RL, DNS at 100ml/hr
3. Inj. Pan 40mg IV BD
4. Inj. Tramadol 1amp in 100ml NS IV/ BD
5. Inj. Thiamine 200mg in 100 ml NS IV/ TID
6. Oint. thrombophobe L/A
7.Monitor vitals 2nd hourly
8. I/O charting
9. GRBS 4th hourly
31.5.2023
Ward :AMC
Unit : 5
DOA : 26.5.2023
30 year male with epigastric pain
S
Yellowish coloured urine
Stools not passed
O:
Patient is conscious coherent and cooperative
Icterus present
No pallor, clubbing, cyanosis, lymphadenopathy , pedal edema
Vitals :
BP- 120/80 mmhg
PR -78bpm
RR-16cpm
Spo2-95% at room air
Temperature - 98.2F
GRBS at 8:00am : 98 mg/dl
CVS: s1,s2 heard ,no Murmurs
RS:BAE ,NVBS,
P/A: soft, non tender, no organomegaly
A:
Acute pancreatitis
P:
1. NBM till further orders.
2. IVF- NS, RL, DNS at 100ml/hr
3. Inj. Pan 40mg IV BD
4. Inj. Tramadol 1amp in 100ml NS IV/ BD
5. Inj. Thiamine 200mg in 100 ml NS IV/ TID
6. Monitor vitals 2nd hourly
7. I/O charting
8. GRBS 4th hourly
9. Oint. Thromphobe L/A
01/06/2023
Ward :AMC
Unit : 5
DOA : 26.5.2023
30 year male with epigastric pain
S
No fresh complaints
O:
Patient is conscious coherent and cooperative
Icterus present
No pallor, clubbing, cyanosis, lymphadenopathy , pedal edema
Vitals :
BP- 120/80 mmhg
PR -76bpm
RR-16cpm
Spo2-95% at room air
Temperature -98.2F
CVS: s1,s2 heard ,no Murmurs
RS:BAE ,NVBS,
P/A: soft, non tender, no organomegaly
A:
Acute cholecystitis with cholelithiasis
P:
1. Oral sips allowed- clear fluids if tolerated- coloured fluids.
2. IVF- NS, RL, DNS at 75ml/hr
3. Inj. Pan 40mg IV BD
4. Inj. Tramadol 1amp in 100ml NS IV/ BD
5. Inj. Thiamine 200mg in 100 ml NS IV/ TID
6. Monitor vitals 2nd hourly
7. I/O charting
8. GRBS 4th hourly








Comments
Post a Comment