This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
—
This is a case of an 80 year old male who came with a chief complaint of fever and chills since 10 days.
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 10 days ago. Then he developed fever with chills insidious in onset and gradually progressive.
He remarked he had burning micturition few days ago. Frequency was normal and there was no change in colour or odour or volume.
He went to a local doctor and was prescribed antipyretics. He was also told by that doctor that he had “pus in his urine” after taking and testing his urine sample. He was also given an injection.
The patient then came to our hospital and was admitted 4 days ago.
The patient also complains of not being able to swallow solid food. He is not willing to eat as it's uncomfortable. He feels his throat is constricted when he’s swallowing food. He is able to drink and swallow liquids.
He also complains of thirstiness and that his mouth feels completely dry despite drinking water. His tongue also appears to be swollen according to the attenders. He also has difficulty in speaking and speaks slowly
He is not able to walk at all since the onset of fever and complains of generalised weakness. He can barely sit up and requires help. The patients attenders also remarked that he seems more lethargic than before
He has not passed stools since being admitted to the hospital.
He also started complaining of epigastric pain today.
He does not complain of nausea, vomiting, headache, body pains, shortness of breath
PERSONAL HISTORY
Daily routine of the patient
The patient’s attenders have reflected that he is a cheerful and an active person in general.
He wakes up at 5 am freshens up and then goes outside to bring milk. He walks a distance of 1 kilometer everyday in the morning to bring milk. He then does household chores like boiling water and then drinks tea and goes by 7 am to the forest for work. His work consists of chopping branches/sticks, carrying and then tying the sticks together and loading them into trucks. He comes back by 10 am and has porridge(containing jowar and ragi). He then rests until lunchtime. His diet consists of rice and vegetables and sometimes meat. After lunch he interacts with everyone and passes time with his family. Evening he drinks tea and goes outside and chats with his neighbours until dinner time. He has dinner and sleeps by 9 pm
5 years before he worked as a watchman in an apartment and did all sorts of miscellaneous work apart from his watchman duties
Diet: mixed
Appetite: decreased since onset of fever
Sleep: adequate
Bowel: Has not passed stools since Saturday
Bladder: regularly passes urine
Addictions: He said that he drinks once or twice a week about 70 mL.
He also smokes around 2-3 beedis per day. He has been smoking and drinking since the age of 20
PAST HISTORY
The patient said he had surgery 5 years ago because he was not able to pass urine properly. Most likely it was BPH and TURP was done
He was also incidentally diagnosed with diabetes and has been on medication since then
He was also diagnosed with hypertension and on regular medication since then.
No history of any epilepsy, asthma, thyroid disorders
TREATMENT HISTORY:
Metformin 500 mg
Glipizide 5 mg
Atenolol 50 mg
GENERAL EXAMINATION:
ABDOMINAL EXAMINATION
INSPECTION
Shape - Scaphoid, with no distention.
Umbilicus - Inverted
No scars, sinuses, engorged veins, no visible pulsations
PALPATION
Soft
Tenderness in epigastric region. Pulsations could be felt in epigastric region
No organomegaly evident
PERCUSSION
Fluid thrill and shifting dullness absent
AUSCULTATION
Bowel sounds present.
CNS EXAMINATION
HIGHER MENTAL FUNCTIONS:
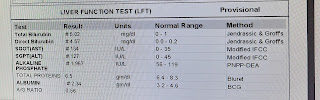
INVESTIGATIONS:
On 26-11-2022 :
On 27- 11-2022:
On 28-11-2022:
On 29-11-2022:
30-11-2022:
1-12-2022:
CULTURE AND SENITIVITY OF URINE SAMPLE:
TREATMENT:
Inj Pentaz 4.5 gm IV stat
Inj KCL 2 amps in 500 ml NS
Tab doxy 100 mg/po/bd
Tab pan 40 mg/po/bd
Inj optineuron 1 amp in 100m NS
Lactulose



























































Comments
Post a Comment