This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Chief Complaints:
Patient had an episode of seizures and lost consciousness on June 22nd night
He complained of generalised weakness since morning
History of Presenting Illness
Daily routine of the patient: Patient wakes up at 4:30 AM and completes his daily activities. He usually does not have breakfast and then goes to work as a labourer at 7 AM. He carries heavy loads and then has a break in the afternoon.He usually does not have lunch and goes to a vegetable stall and carries loads again. He says he consumes alcohol about 90-360 mL almost every day depending on how much money he has. He comes home around 7 and has dinner and sleeps.
Patient was apparently asymptomatic 10 years ago and then he started consuming alcohol regularly. He says he experiences restlessness and sleep disturbances if he is not consuming alcohol
Sequence of events that lead to the present day:
He was not feeling well since the past 2 days and had 2 episodes of vomiting and decreased food intake. He was resting the whole day and at night he wasn’t able to sleep he got up and lost consciousness, and has no recollection of events. Patient’s attender who witnessed the episode, said the patient fell on the ground and had an episode of seizure which lasted for 5-10 minutes, tonic clonic movements of upper and lower limbs.
Past history:
He had a history of a similar episode of seizure in the past, for which he was taken to the local RMP for treatment and came home afterwards.
Personal History:
Diet: mixed
Appetite: decreased
Sleep: experiences disturbances
Bowel and Bladder: normal
Habits: known alcoholic since 10 years.
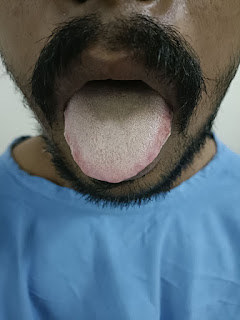
General Examination
Patient is conscious, coherent and cooperative.
BP;30/90
PR: 86 bpm
RR: 18/min
Pallor is present. No cyanosis, clubbing koilonychia, lymphadenopathy, edema
MOTOR SYSTEM :
Right Left
Bulk:
Inspection. N. N
Palpation. N. N
Tone:
UL. N. N
LL. N. N
REFLEXES
B T S K A P
R 2+ - - - - Flexor
L 2+ - - - - Flexor
CEREBELLUM:
Walking in a straight line:
Dydiadochokinesia:
Romberg test:
Investigations:
DIagnosis:
Seizures secondary to alcohol withdrawal





Comments
Post a Comment